The official U.S. government website for Medicare provides a tool that allows consumers to compare information about nursing homes. It is called Nursing Home Compare, and contains quality-of-care information on every Medicare- and Medicaid-certified nursing home in New Jersey and Pennsylvania.
The tool creates that information based on the “skilled” care that nursing homes provide, which is care given when you need skilled nursing or rehabilitation staff to manage, observe, or evaluate your health status. For example, skilled care includes intravenous injections and physical therapy.
The “Overall 5-Star” Rating System
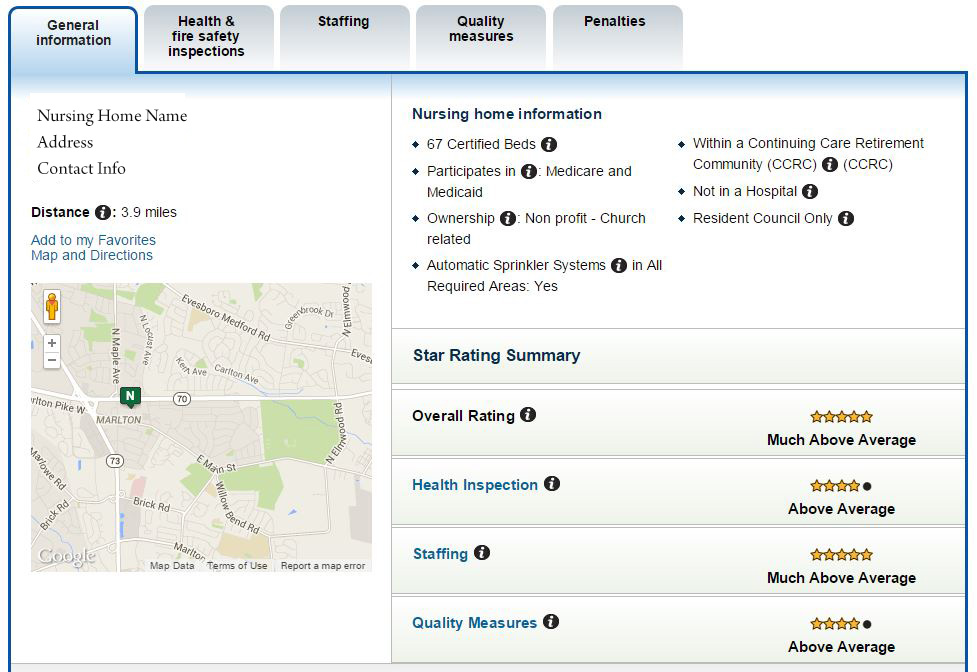
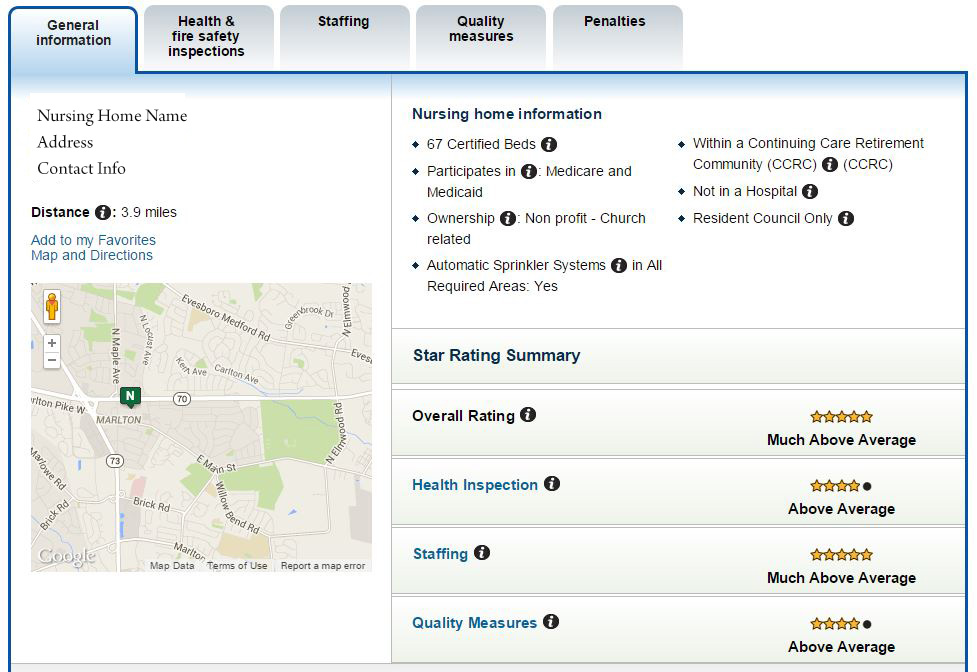
To rate the nursing homes, the tool uses an “Overall 5-Star” rating system. It assigns 1 to 5 stars, with more stars indicating better quality, across three “domains.” Those domains include: (1) Health Inspections, (2) Quality Measures, and (3) Staffing. The tool reports the ratings in table or profile form. Here is example of a nursing-home profile:
The Domains
The tool generates the rating for the Health Inspection Domain based health-inspection ratings from the three most recent annual-comprehensive inspections, and inspections instigated in response to complaints in the last three years. It places more emphasis on recent inspections.
It generates the rating for Quality Measures Domain by combining the values on 9 out of 19 Quality Measures. Some of those measures include, for example:
- the percentage of long-stay high-risk residents with pressure ulcers;
- the percentage of long-stay residents experiencing a fall with major injury; and
- the percentage of long-stay residents who self-report moderate to severe pain.
The tool derives those values from clinical data that nursing homes regularly report on a form called the Minimum Data Set.
And finally, the tool generates the rating for the Staffing Domain based on (1) the Registered Nurse (RN) hours per resident day, and (2) the “total staffing” hours per resident day. Total staffing includes: RNs, Licensed Practical Nurses, Licensed Vocational Nurses, and Certified Nurse Assistants. Nursing homes report staffing hours, which are from a two-week period just before the state agency conducts an inspection, to the New Jersey or Pennsylvania state-inspection agency. The agencies, in turn, report those data on Nursing Home Compare.
At Stark & Stark, our nursing-home negligence lawyers dedicate their entire practice to prosecuting nursing-home negligence lawsuits. We highly recommend the Nursing Home Compare tool when trying to assess a nursing home’s quality.